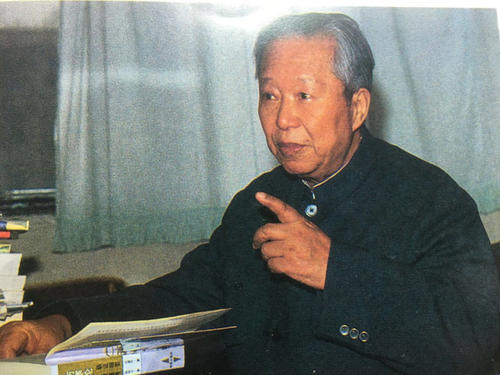
With my upcoming Liú Dùzhōu book release, I felt it would be apt to share a couple random cases from this brilliant physician. These cases do not appear in my book, but were ones I found during my many deep dives and Liú Dùzhōu rabbit holes. Enjoy!
Case of Dysmenorrhea
Patient: Li, female, 45 years old. Initial consultation on May 5, 1993.
History:
The patient developed dysmenorrhea one year prior after undergoing an induced abortion. During each menstrual period, she experienced severe, cold pain in the lower abdomen that was unrelieved by analgesics. Her menstrual cycle was delayed, with scanty, dark-colored blood containing clots. This menstrual period began yesterday. She also presented with dry mouth, chapped lips, dizziness, soreness in the waist, weakness in the legs, and fatigue when lifting. The tongue was dark, and the pulse was deep.
Diagnosis:
This was diagnosed as a condition of deficiency and cold in the Chong and Ren channels, with blood stasis obstruction.
Treatment:
The treatment principle was to warm the channels, dispel cold, eliminate blood stasis, and nourish the blood. The prescription was derived from the Jīnguì yàolüè formula Wēn Jīng Tāng:
wüzhūyú 8g
guìzhī 10g
shēngjiāng 10g
dāngguī 12g
báisháo 12g
chuānxiōng 12g
dǎngshēn 10g
zhìgāncǎo 10g
mǔdānpí 10g
ējiāo (dissolved separately) 10g
bànxià 15g
màidōng 30g
Outcome:
After taking five doses, the cold pain in the lower abdomen was significantly relieved. The same prescription was continued for five more doses. By the next menstrual period, the abdominal pain did not recur. From that point forward, her menstruation became regular and without discomfort. (Selected Clinical Case Studies of Liú Dùzhōu)
Commentary:
Wēn Jīng Tāng is effective for treating dysmenorrhea. Renowned Hangzhou physician Qiu Xiaomei once recalled:
“I was fortunate to work alongside the famous Zhejiang physician Ye Xichun. Ye’s profound and unique medical skills provided me with many valuable insights. For example, when treating cold-induced dysmenorrhea, the routine application of Wēn Jīng Tāng often proved effective. However, there were cases where it was ineffective.” (The Path of Renowned TCM Physicians)
This highlights that even when using Wēn Jīng Tāng, it is crucial to match the formula to the correct pattern. In this case, Dr. Liú Dùzhōu documented not only the patient’s localized symptoms (such as delayed menstruation, severe cold pain in the lower abdomen, and scanty dark menses) but also systemic characteristics such as dry lips, a dark tongue, and a deep pulse, along with the abortion as the inducing factor.
Case of Neurotic Disorder and Irritability
Patient: Cao, a 72-year-old female, who first consulted on October 26, 1995.
The patient had been experiencing persistent irritability for two years, with a recent worsening trend.
Western medicine diagnosed it as a neurotic disorder, and she was given sedatives and anxiolytics, but there was no improvement. She then sought traditional Chinese medicine treatment.
Presenting Symptoms: The patient complained of intense irritability, which was unbearable. Her family members were sympathetic and cautious, but she could not express herself or felt misunderstood. She became agitated and, during severe episodes, felt relief only after hitting her chest and abdomen with a stick. She felt a rising sensation from the navel to the chest, which worsened the irritability. She also experienced abdominal bloating with a feeling of obstruction. Additional symptoms included insomnia, restlessness, nausea, poor appetite, irregular bowel movements, and yellow urine. Her tongue was red at the tip, with a greasy coating, and the pulse was wiry and slippery.
Diagnosis: A pattern of fire stagnation in the chest and abdomen, with downward pressure on the stomach and intestines.
Treatment Strategy: Soothe stagnation, clear heat, regulate qi, and reduce fullness.
Prescription: Zhīzǐ Hòupò Tāng
zhīzǐ 14g
zhǐshí 10g
hòupò 15g.
7 doses.
Follow-up: After 7 doses, the patient reported a 50% reduction in irritability. Her chest and abdomen felt clearer, and her mood stabilized. She was able to sleep at night, and her appetite improved. The treatment was highly effective, and the patient continued with 7 more doses. Upon follow-up, she still had symptoms of sleep disturbances, dry mouth, a bitter taste, and yellow urine, indicating that heat had not fully resolved.
The prescription was then changed to Chái Qín Wēn Dǎn Tāng [Wēn Dǎn Tāng plus cháihú & huángqín) combined with Zhīzǐ Hòupò Tāng to clear phlegm-heat and treat the remaining symptoms. After one month, the patient fully recovered.
(From Liú Dùzhōu Lin Zhen Yan An Xuan (Selected Clinical Cases of Liú Dùzhōu))
Note: The difference between Zhīzǐ Hòupò Tāng and Zhīzǐ Shí Tāng lies in the abdominal symptoms. The former is indicated when abdominal symptoms like bloating and constipation are present, while the latter is primarily used for chest-related symptoms like chest oppression and cough. Zhīzǐ Hòupò Tāng and Xiǎo Chéng Qì Tāng both contain zhǐshí and hòupò, which treat abdominal fullness and pain. The key difference is that zhīzǐ and dàhuáng have distinct effects: Zhīzǐ clears irritability, while dàhuáng is used to purge and clear heat. Therefore, Zhīzǐ Hòupò Tāng is more suitable for chest obstruction and irritability, while Xiǎo Chéng Qì Tāng is better for constipation and abdominal pain. The patient’s detailed symptoms of irritability and abdominal fullness illustrate the application of Zhīzǐ Hòupò Tāng for heat-related disturbances and its ability to address both physical and emotional symptoms.