杨大华. 汉方治验选读
慢性肝炎(矢数道明治验)
48岁妇女,5年前发病。由于有胸不适,右肩酸痛,右颈部肿,右手麻木,微热持续不退,在大学附属医院诊察,诊为急性结核性淋巴结炎,进行了链霉素和对氨基水杨酸钠治疗。 但又引起剧烈的胃障碍,出现严重黄疸,甚为惊恐,又住入其他医院诊为急性肝炎,2个月后出院。
Case taken from “Selected Readings on the Efficacy of Kampo Formulas”, by Yang Dahua
Chronic Hepatitis (A Case by Dōmei Yakazu)
A 48-year-old woman developed symptoms five years ago. She experienced chest discomfort, right shoulder pain, swelling in the right side of her neck, numbness in her right hand, and persistent mild fever. After being examined at a university-affiliated hospital, she was diagnosed with acute tuberculous lymphadenitis and treated with streptomycin and para-aminosalicylic acid. However, this led to severe stomach problems and the onset of serious jaundice. Alarmed, she was admitted to another hospital and diagnosed with acute hepatitis. After two months, she was discharged.
此后5年来,右肩酸痛,右手麻木,浮肿一向不治,过劳淋巴结立即肿大。又胸中苦于胀满,裤带一勒紧即感恶心。 体格、营养状态一般,面色尚可,脉弱,血压正常。心下紧张如板状,有剧烈压痛,右季肋下痛尤为明显。肩酸痛严重时有短气。
Over the following five years, her right shoulder pain, hand numbness, and swelling remained untreated. Her lymph nodes would swell with overwork, and she suffered from a persistent feeling of distention and fullness in her chest, with nausea when tightening her belt. Her physical condition and nutrition were average, her complexion was decent, and her pulse was weak but her blood pressure normal. She had tightness below her chest like a hard plate with intense tenderness on palpation, as well as quite noticeable pain below her right ribs. When the shoulder pain was severe, she would experience shortness of breath.
以上所见正与“心下急,郁郁微烦,胸胁苦满,心下痞硬,呕吐,腹满痛”之大柴胡汤条文几乎一致。由于右肩酸痛与右手麻木、右季肋紧张压痛相互关联,故胸胁苦满有时轻快,有时不轻快。尽管脉较弱,仍与大柴胡汤加葛根5g。 服用本方10日,5年来之肩酸痛、右手麻木、胸闷不舒,几乎痊愈。1个月后,乘汽车、电车晕车亦消失,心下痞硬和苦满等症状好转。服用3个月,宿疾一扫而光,停药。(《临床应用汉方处方解说》)
The symptoms observed closely align with the [Original] line of Dà Chái Hú Tāng [from the Shang Han Lun]: “Distress below the heart, a feeling of depression and slight vexation, fullness in the chest and rib-sides, hard glomus below the heart, vomiting, and abdominal fullness and pain.” Because of the connection between the right shoulder pain, hand numbness, and the tightness with tenderness below the right ribs, the fullness in the chest and rib-sides would fluctuate, sometimes improving and other times remaining unchanged. Although her pulse was relatively weak, Dà Chái Hú Tāng was prescribed with the addition of 5g of gé gēn (Pueraria root).
After taking this prescription for 10 days, the shoulder pain, hand numbness, and chest discomfort she had suffered with for five years was almost completely resolved. A month later, her motion sickness while traveling in cars and trains also resolved, and her hard glomus below the heart and fullness improved. After three months, her long-standing issues were completely resolved, so she discontinued the herbs. (Explanation of the Clinical Applications of Kampo Formulas by Dōmei Yakazu).
剧烈的胃障碍,出现严重黄疸”要考虑对氨基水杨酸钠的不良反应。诊为急性肝炎不恰当,应该是药物性肝损更为合适。停药及治疗后恢复正常,此后5年来的一切不适与肝损无关。“心下紧张如板状,有剧烈压痛,右季肋下痛尤为明显”,这些腹证也不是肝脏疾病的表现。
The severe stomach disturbance and jaundice should be considered an adverse reaction to para-aminosalicylic acid. Diagnosing it as acute hepatitis was inappropriate, [whereas] drug-induced liver damage would have been more accurate. After stopping the medication and undergoing treatment, her condition returned to normal, and her discomfort over the next five years had nothing to do with liver damage. The phrase “tightness below the chest like a hard plate, with intense pain on palpation, as well as quite noticeable pain below her right ribs” does not indicate symptoms of liver disease.
患者的大柴胡汤证非常典型,因此抛开肢体症状独取腹证。加葛根可能是兼顾“右肩酸痛,右手麻木”的肢体症状。如果不加葛根,是否也一样有效?既然认准是大柴胡汤证,就没有必要加葛根。且大柴胡汤加味药多为芒硝、厚朴,加葛根则为少见。
The patient’s case was a typical presentation of Dà Chái Hú Tāng, so it was appropriate to prioritize the abdominal symptoms without giving much attention to the limb symptoms. The addition of gé gēn was likely to address the limb symptoms of right shoulder pain and hand numbness. However, would the formula have been equally effective without adding gé gēn? Since the formula aligned with the Dà Chái Hú Tāng pattern, adding gé gēn might not have been necessary. It is also not common to add gé gēn to Dà Chái Hú Tāng, whereas herbs such as máng xiāo or hòu pò are more common.
脉弱,依然用大柴胡汤,体现了重腹证、轻脉象的理念。大柴胡汤证体现在慢性病中,脉象的反应有可能不像急性病那样强烈,也就是说,当脉象与腹证不一致时,需要舍脉从腹证。《重要汉方处方解说口诀集》(邱年永翻译)说“大柴胡汤证之脉为沉实或沉迟而有力是正证,但不必拘泥此种脉象”。并举例痈疽、下利、温病等出现大柴胡汤证时脉象等变化。也就是说,大柴胡汤证等腹证相对稳定,但脉象可以因疾病的不同而有个体差异。
The decision to use Dà Chái Hú Tāng despite the weak pulse reflects a preference for focusing on the abdominal signs as opposed to the pulse. In chronic conditions, the pulse may not react as strongly as in acute illnesses. In other words, when the pulse and abdominal signs do not align, it is necessary to prioritize the abdominal signs. The Essential Guide to Key Kampo Formulas: A Collection of Mnemonics (translated by Qiu Nianyong) states, “The pulse for the Dà Chái Hú Tāng pattern is usually deep and excess, or deep, slow and strong, yet [one] need not rigidly adhere to this pulse manifestation.” [The text] also gives examples of variances in the pulse when Dà Chái Hú Tāng is indicated in cases of abscesses, diarrhea, warm diseases, etc. This suggests that the abdominal signs associated with Dà Chái Hú Tāng are relatively stable, while the pulse can vary according to the disease.
患者的大柴胡汤腹证是否为结核性淋巴结炎所致?不得而知。肢体症状均在右侧,右季肋下痛是否与此相关?也许在汉方医生眼中,肢体的症状与腹证都属于同一种病理变化,是一棵树上的叶与花。使用大柴胡汤之后这些表现都得以解除,则大柴胡汤相当于将树连根拔起,花叶俱萎。从本案来看,肢体的症状先消失,腹证则消除缓慢,类似于花与叶的差别。花与叶对营养的需求不同,凋落自然有迟有早。腹证与肢体症状在形成上也并非一致,其成因应该更加复杂。
Was the patient’s abdominal pattern caused by tuberculous lymphadenitis? It is unclear. Her limb symptoms were all on the right side—was the pain below the right ribs related? Perhaps from the perspective of a Kampo physician, the limb and abdominal symptoms could be manifestations of the same pathological change, like leaves and flowers on the same tree. Once Dà Chái Hú Tāng was administered, all these symptoms resolved, suggesting that the formula uprooted the tree, causing both the flowers and leaves to wither. In this case, the limb symptoms disappeared first, while the abdominal symptoms resolved more slowly, akin to the different timing of the leaves and flowers falling. The development of abdominal signs and limb symptoms is not necessarily the same, and their underlying causes are likely more complex.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
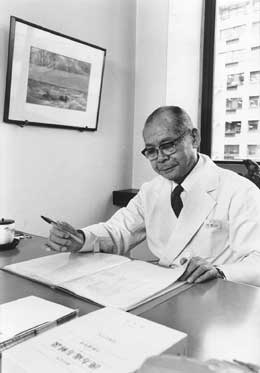
Dōmei Yakazu (1905-2002), was a Japanese physician born in Tokyo. Dōmei graduated from the Tokyo Medical College in 1930 and later studied Chinese medicine. In 1954, he conducted pharmacological research at Tokyo Medical University, obtaining his doctorate in 1959.
For over 50 years, Dōmei Yakazu, together with Keisetsu Ōtsuka, dedicated himself to the revival of Kampo (traditional Japanese medicine) in Japan, making significant contributions to the promotion and development of Eastern medicine. His notable works include; Explanation of Key Kampo Formulas from Later Generations, Explanation of the Clinical Applications of Kampo Formulas, Practical Kampo Diagnosis and Treatment, The Great Encyclopedia of Kampo Medicine, The Medical Encyclopedia of Kampo Diagnosis and Treatment, A Brief History of Kampo over the Past Century of the Meiji Era, and A Hundred Stories of Kampo Therapy.